Road to Recovery: My ACL Story, version 3
(Last Updated On: )
I’ve thought a lot about where to start this story. Usually you start a story about an injury when the injury occurs. But, I’m not sure exactly when this one happened – and that alone makes this an interesting story. You see, I’ve torn my ACL twice before, one on each knee. In both of those incidents, there was never really any question in my mind that I had torn my ACL. Even though I wanted to deny it, I knew it was gone. So, imagine my surprise when I went to visit the PA of my orthopedic doctor and she said, “Well, now…. I think something might be wrong with your ACL.”

I went through the motions though, getting an MRI, because signs had told me that something was definitely wrong with that knee. In my story of my conundrum on Conundrum I talk about how my knee moved in ways that it should not have during a small fall while skiing. But, I still finished the ski and walked the rest of the way back to the car. In my first two ACL-tearing incidents, there’s no way I could have done that. Of course my ACL must be fine.
 I even texted Frank after the incident that I “tweaked my knee” but that it was “definitely not a ligament.”
I even texted Frank after the incident that I “tweaked my knee” but that it was “definitely not a ligament.”
The days that pass after an MRI are always the worst. I had this disk in my possession that told the story of my knee, a story that was about to unfold. But, the story would not be revealed until my doctor’s appointment which was days later.
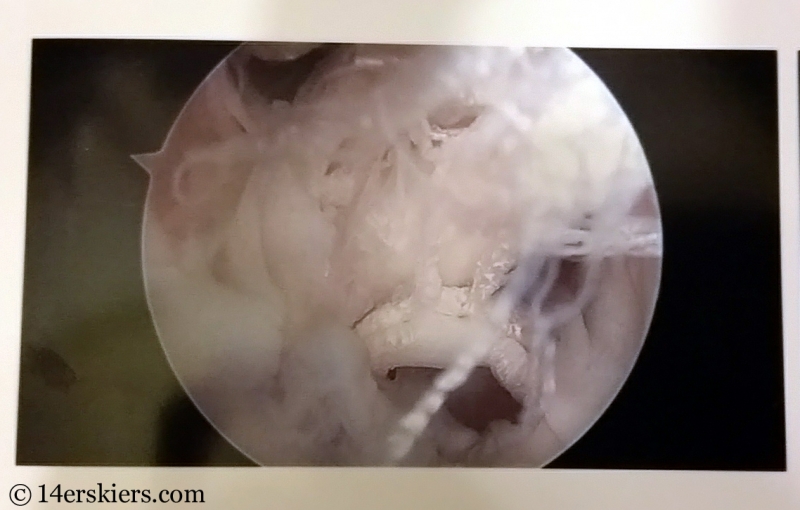
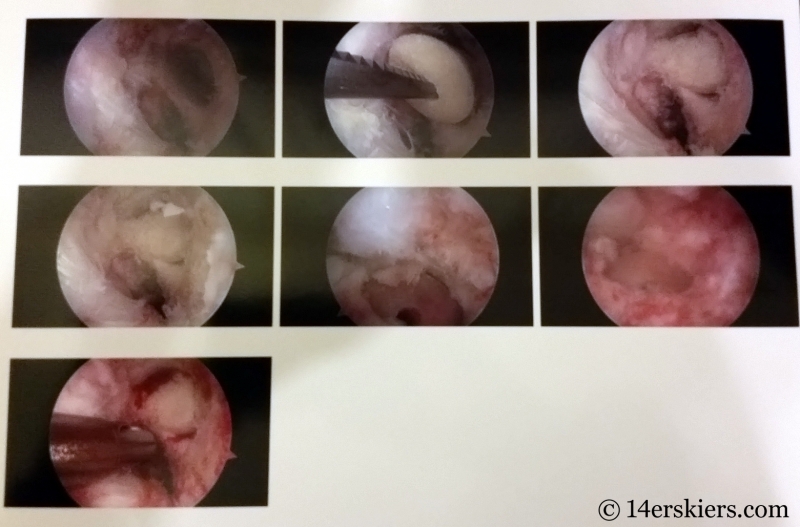
I was nervous when I stepped into the doctor’s office. The orthopedic doctor started bombarding me with questions – Had I fallen lately? How has my knee been feeling? But all I wanted to know was what was wrong with my knee. I kept answers short and finally rudely blurted out, “What did the MRI say? What’s wrong with my knee?” “Your ACL is torn and your meniscus is too.”
“NOOOOOO!” I screamed in disbelief, and immediately broke into tears. Two ACL tears were enough already. It was July, and surgery over the summer might not allow for a full recovery for skiing in winter. All these things rushed through my brain – but mainly that it was looking like I was going to be missing a big chunk of ski season. And I knew that a second ACL repair on a knee was never as easy as the first…
Version 1
Perhaps the way I should have started the story is with my first ACL injury. It was close to Memorial Day Weekend in 1997. I was at a training camp with the CU Freestyle Ski Team in Parsenn Bowl at the top of Winter Park Ski Resort. That day, a handful of us were working on perfecting our jumps. We’d jump, take off our skis, hike back up, jump again, and repeat.

As soon as I landed, I screamed. The Winter Park Ski Team, the US Ski Team – they all could hear me screaming. It was one of the most painful things I’d experienced in my life. I had hyper-extended my right knee, and I was fairly certain that I had torn my ACL, and probably some other stuff too.
Less than a month later, I was going under the knife with Dr. Sterett who was practicing with the Steadman-Hawkins clinic at the time. We chose a patellar-tendon autograft for the repair. There is a story of recovery to tell with version 1 of course, but after working very hard at getting strong, I was skiing just 5 months after surgery.
Version 2
I felt it as I landed – that “pop” in the knee. That “pop” that every skier hears about, and every skier dreads.

I was coaching an all-woman’s ski clinic and we had been practicing cliff-jumping. After a long pause, one of the ladies shouted out from above, “Are you okay?” “Um, no. I think I just blew out my knee,” I said very matter-of-factly.
This time it was my left knee and this repair would be done using an allograft anterior tibialus. I did miss the remainder of the 2009 ski season, but I was skiing again as soon as the snow flew the following fall. But, Version 2 has it’s own story of recovery to tell, much of which I have documented on this blog. Recovery is never really very easy….
Version 3
And that circles me back to this story. Version 3 I’m calling it. My left knee is again devoid of an ACL and this time, I’m not really sure how it happened. Maybe it was that slip I took while shouldering my skis while hiking out of Park Cone back in April? Or maybe it was when my ski got caught under that log a few seasons back? Or that tweak my first season back after Version 2 while skiing the East Face of Gothic? Or maybe the allograft just failed and I never realized?
What I do know is that Version 2’s repair never felt right – it always felt a little loose, a little bit weak, a little “off”. Version 1 crunched around and grinded a lot due to the patellar tendon slice that was taken out to use as the graft for my ACL, but the knee itself always felt strong. I never questioned it’s stability.
So, after getting hit over the head with the news that my ACL was once again gone in my left knee, I took some time over the next day to rationalize and question things. Why did the Version 2 repair never feel right? Was it because it was an allograft? Did the allograft fail during rehab? Was the graft placement in my knee done wrong which would increase my chances of re-tearing it? Why was my doctor suggesting allograft again? Was this really the right choice?
The Search
A physical therapist friend of mine encouraged me to get a second opinion on my knee. So I did. With the same MRI and the same physical exam, that doctor told me that my ACL was only partially torn and that my meniscus was probably fine.

So, I sought out a third opinion…. and there I was gallivanting all over the state to find the right surgeon for me.
What I learned was that orthopedic doctors are consistently inconsistent. While the one doctor who said I had only a partially torn ACL and no meniscus tear was definitely the outlier in the bunch, each surgeon had his or her own suggestions for how to repair my knee. For example, most doctors said I would probably need a bone graft to repair the tunnels created from my previous repair. One said I would not. But, even how they would do the bone graft varied – one said he would take autograft cores from my hip, another one said they’d use allograft “bone paste”, and the last one said he’d use allograft cores. Still, there were some over-arching consistencies – most of them agreed I probably needed staged surgery (bone graft surgery first) and that the prior repair that had been done in my left knee was too posterior and that likely increased its chances of failure.
And I haven’t even gotten to the actual type of graft yet… Or the meniscus, or how they would handle rehab. All of those are other chapters to this Version 3 story….
I finally decided, after my 5th visit to various orthopedic doctors, that Dr. Vidal of CU Sports Medicine was the right fit for me.
Advice for Finding the Right Orthopedic Surgeon
After tearing my ACL for the third time, I feel that I’ve gained some valuable experience that I wish to pass on about finding the right orthopedic surgeon. I got lucky with my Version 1 surgeon. But, I wish that someone had really made me do these things before I rushed into surgery with my Version 2 doctor:
- Research – Take time to research BOTH your doctor and the kind of ACL repair technique you want done. These things go hand in hand, as some doctors are more experienced in certain repair techniques than others. You’ll not only want a doctor who has a successful track record for surgeries, but who also is competent in the repair technique you want to use. At the same time though, your surgeon may suggest a technique that you may come to like.
- Get Multiple Opinions – As I said, one thing I learned from visiting 5 orthopedic surgeons in a few weeks was that they are consistently inconsistent. But, there’s also some reigning consistencies too. It’s good to get a variety of opinions, from diagnosis to surgery options and even rehab techniques.
- Come with a list of questions – You’ll think you’ll remember all the questions you want to ask, but you probably won’t. It’s good to built a list of questions so you don’t forget. if you think of other questions during the appointment, write them down, so you remember to ask these questions to other doctors you may choose to visit. The questions I asked were things like: What would you suggest for my graft options? Is autograft really that much more successful that allograft? What autograft options should we be thinking about? Will I need bone graft surgery? Where will the bone grafts come from? How will you repair my meniscus? What will my rehab be like for the first surgery? The second? When will I be able to ski again?
- Take Notes – After the 4th doctor, I started to get them confused. Which doctor told me I’d be in a straight leg brace for 6 weeks? Wait, the other one said only 3 weeks? Which one was that. How long did they say I needed to wait before I could have my second surgery after the bone graft? You see my point…..
- Take Charge – Don’t just let a doctor tell you what to do. Ask questions, ask other doctors, research on the internet, ask your physical therapist (they see what is successful and what is not and are usually not afraid to share). Ultimately, you want to be armed with information so that you can make decisions for yourself and feel good about the choices you have. The most important decision is finding that surgeon that you feel is the right fit for you, both with surgery and recovery techniques, both of which can vary widely. I found the orthopedic surgeons to especially differ with techniques surrounding bone grafts, cartilage repair, or meniscus repair. Keep in mind, that some decisions will need to be made on the fly while you’re under during surgery. You’ll want to have faith that your surgeon will make a choice that you’ll agree with.

There is nothing better than going into a surgery knowing you have full faith in your doctor and what he or she will do for you. So, even though you’ll want to rush into surgery right away to begin the recovery process, it’s worth the extra couple of weeks it takes to do it. Remember, these are your only knees. You want what’s best for them!
Version 3 Status

While my knee still swells up after a long day on my feet, I am doing day to day activities as normal. I began riding a stationary bike 2 days after surgery, riding on roads a week later, and have now returned to singletrack in just the last couple of days.
I still don’t have an ACL. I still have a torn meniscus. Skiing is not really recommended as I could do further damage to my knee. They are especially concerned about further damage to the meniscus. A torn meniscus is prone to more tearing, and currently the meniscus looks like it is repairable. Further damage could compromise it enough so that it may no longer be repairable.

I don’t have a date set yet for my second surgery, but it will likely take place during the mid to end of November. Believe me, I’ll be ready to get the healing process really started. I am told it will be 9 months after my second surgery before I can ski again.
For now, I remain in limbo… able to do a lot. But, not the one thing I really want to do – which is ski. I won’t have a ski season, and that continues to sadden me to no end. Still, I try to focus on the fact that I will be skiing again, and that I will come back stronger than ever, just like I’ve done before.
And for now, I get to enjoy biking with yellow aspen leaves flying all around. After all, fall is my favorite time to ride 🙂
- Mount Buckskin (17 May 2020) - May 28, 2020
- Horseshoe Ski (14 May 2020) – The mountain whose journey nearly killed me - May 27, 2020
- Sayres X-Rated Ski (10 May 2020) - May 19, 2020



Wow, sweating just reading about it. Your story conveys a great spirit and attitude that will go a long way towards pumping up your recovery. I blew out my ACL at age 47. 14 years and many mountain climbs, ski days etc., the knee remains solid and strong. Had (2) choices at the time: patellar or 3rd hamstring (weak) tendon. Chose the hamstring tendon. Ever since, a slight degradation in hamstring muscle size and strength…say 10% strength loss and 15%-20% muscle size loss. I do heavy strength training and can see/feel effect. It is not enough to stop anything I do nor worry about. On the other hand, my knee usage and performance are 100% with no degradation in knee stability, flexibility and range of motion. No onset of arthritis either. The one and only negative outcome thus far is I chose to hang up my soccer cleats.
They are using cadaver tendons for ACL reconstruction. My general physician had his done that way. He said it took 4 months to be back at it. The rehab time is much less, as well as less muscle mass and strength loss. That makes sense, not healing in two places.
Congratulations on your ski mountaineering accomplishments. Very cool. Hope you are back in action real soon. As a beginner in BC skiing, I appreciate your sharing of BC ski opportunities around Colorado.
Yes Uwe, I had my 2nd repair done using an allograft. Although the pain was much less and getting back to things was easier, the recovery is actually considered by most orthos to be longer because it takes more time for the graft to heal and grow a sheath and blood supply that prevents tearing. 4 out of the 6 orthos I visited highly recommended autograft in my case due to my failure of the allograft and how active I am. Although low, the failure rate of allograft is still 3 times more than autograft, and there are new studies that show that allografts tend to fail even more so years down the road. So, for this repair, I am returning to an autograft solution in hopes that I will never need ACL surgery again!