Unlucky Lucky – Part 3 – The most painful surgery
(Last Updated On: )
After spending a week in ICU, it was so good to be on the regular trauma floor. The wake ups in the middle of the night were less frequent. I actually had a closed off bathroom with a shower. I didn’t have nearly as many IV’s and electrodes connected to my body. I had been doing walking laps around the ICU, being escorted by physical therapists or nurses, but on the regular floor, I was allowed to be escorted by friends and family. Walking, and therefore healing, was easier.

I was visited by many more friends and family, and also hospital staff and volunteers that gave me massages or sang or played music. Mollie the dog even gave me a dose of healing magic.

I was even visited by a trauma survivor, who was a volunteer for a peer support group for trauma survivors like me. It was great to be able to connect and share our stories and gain advice for how to recover from this experience, both physically and mentally. The Trauma Survivors Network is a great resource.
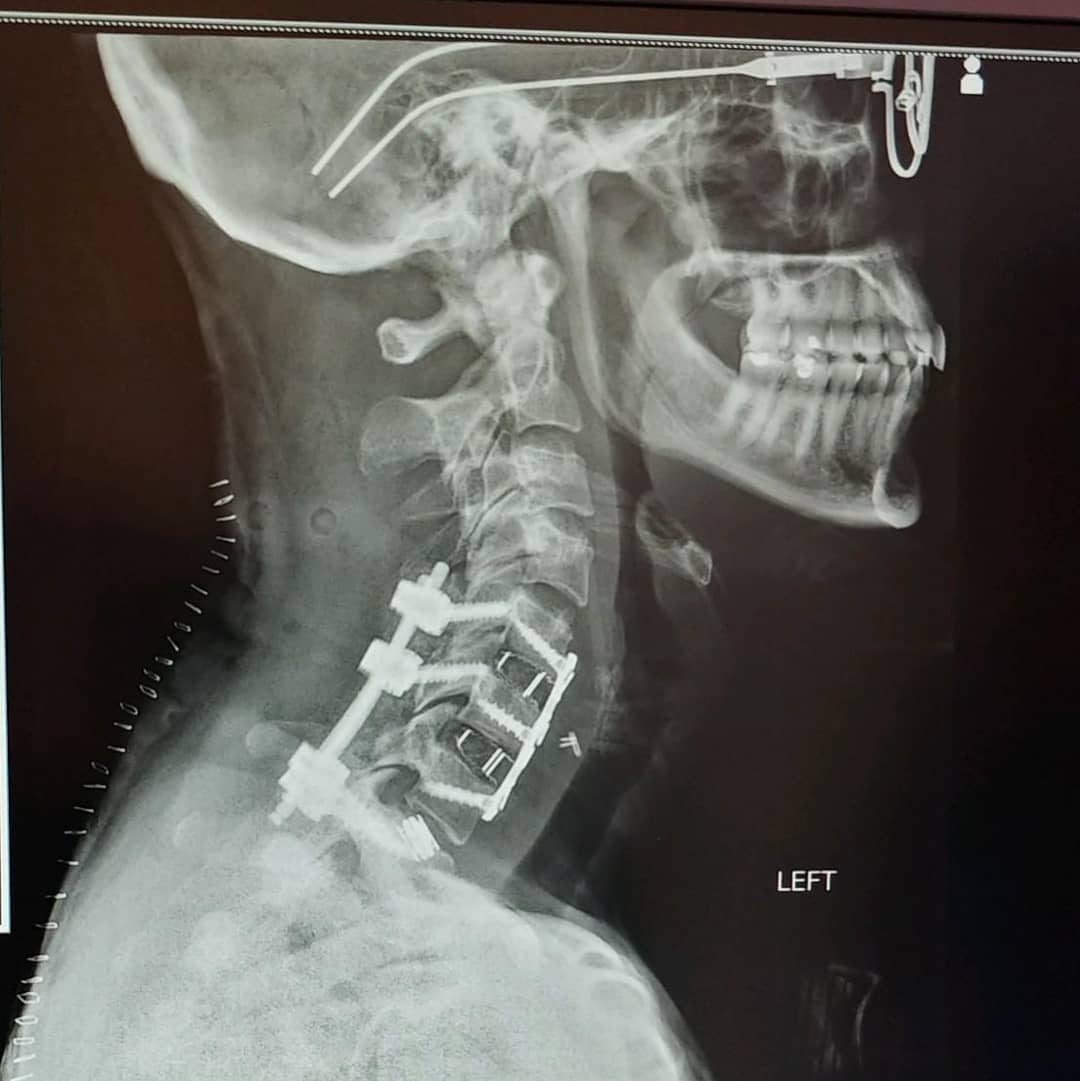
I was honestly feeling pretty good, but I remained the hospital largely because I still had one more surgery to go. The day after my admission to St. Anthony’s Hospital, they had operated on my cervical spine, stabilizing it from the front. But, the still wanted to stabilize it from the back. Tuesday July 16th was the day slated for that surgery.
On Monday night, I was alone in my room and my spine surgeon came in to visit with me. Some surgeons can be weird, and admittedly, this was one of them. He said that this surgery was going to be painful – more than the last spine surgery, that it might make me worse, and that he would pray for me. I’m sure he was going from and “under-expect but over-perform” standpoint. But, his words didn’t inspire confidence in any way. I would have preferred to hear something like, “You know, there are risks with this surgery, but I have had overwhelming success in similar surgeries” – Or something along those lines. Instead, his words were making me squeamish and more nervous than I already was.
But, as I have said before, the Universe seems to send you the things you need when you most need them. Moments after my surgeon left, I was visited by a trauma PA whom I had not met before, but he was the husband of a former roommate and ski teammate from college. He knew details of my case, told me he was impressed by my positivity and recovery, and was able to answer some questions for me. I had been asking various hospital staff if there was a possibility we could see if my ACL on my left knee was intact, as I had a history of tearing it before. My last surgery for it was just in 2016 and it had taken me a year to recover. This PA was able to perform the Lachman’s test on me to determine that yes, the ligament was indeed intact and feeling strong. Whew. After his visit, I felt confident again, and slept more soundly again.
My surgery was scheduled for 7:30 am. I woke up early and ready for what should be my last surgery for this hospital stay.
As they wheeled me down toward the operating room, I continued to be nervous. I remember meeting various nurses and PA’s who would help during the surgery, the lights and smells and sounds of the OR. And then, before I knew it, I was waking up in post-op, and it was already 3 pm.
They held me in post-op for quite some time because my blood pressure was low. But, it’s always low, I tried to tell them. I was trying to minimize the opioid drugs for pain, as I don’t typically like how they make me feel, and most of them tend to make me nauseous yet do nothing for the pain. But ended ended up giving in to one shot of it in the IV. It turns out the surgeon was right, it turn. It hurt A LOT.
They wheeled me up to my room where I had another restless night of sleep, and a whole lot of pain. I finally had to give in to narcotics again. Through the night, they gave me several IV doses of Dilaudid. This is one opioid I have had success with in actually helping pain, without making me nauseous. But, I did’t like the doses they gave me through the IV as they were strong and made me pretty loopy.
The next day I remained in a lot of pain, but tried to stay off the Dilaudid. But, I was miserable. Anyone who knows me knows that I have an incredibly high tolerance for pain. I endured three knee surgeries, a thyroid surgery, and a thumb surgery without taking opioid pain meds post-op. Even from this trauma event alone, breaking a femur is supposed to be very painful. Yet, I barely complained about it. But this surgery. This surgery was the most painful one I’d had to date.
The nurses tried putting me on oral Percocet which again did nothing for the pain, but made me nauseous. And my pain level continued to be untolerable. I needed to get it under control. Eventually, I elected to be put back on a Dilaudid pain drip, where I could press a button as often as every 10 minutes to release los doses of it into my IV. I preferred these low doses because I didn’t feel so loopy, yet the pain was managed. Almost instantly I was feeling much better.
That night I slept well, no longer in severe pain. I don’t think I even used the pain drip for 12 hours. I think had them try a new oral medication, Tramadol, which again seemed to keep my pain at bay without making me nauseous. This was important step for me, as in order for me to be discharged, they needed my pain to be under control with oral pain meds.
Things were looking up, and it was looking very possible that I might be discharged the very next day. There were still two things that needed to happen before I could be discharged. First, I needed to show the physical therapists I could walk up and down stairs – which I hadn’t been able to do because I had been connected to IV heparin blood thinner the whole time. But there was a brief time when I was taken off and they could finally test me:
Next, I needed to transition from the IV bloodthinner to an oral blood thinner, to help control the blood clot that was in my vertebral artery, posing a risk of stroke. I didn’t want to go on Coumadin for multiple inconvenience issues = I would need to get daily blood tests for awhile until the dosage was determined, and then weekly blood tests after that, for as long was I was on the drug, which could be up to 6 months. Since I can’t drive for awhile, this would not only be inconvenient for me, but for my husband. So, we looked for other alternatives and due to insurance reasons, decided on Xeralto.
Finally, agreed it was time for me to go.



While I had left the hospital, it wasn’t time for me to go home yet. We decided it would be best for me to stay in Golden with Frank’s family for a few days. We had a follow up for the femur on Tuesday and my parents, who were visiting from Ohio, weren’t planning on leaving until Sunday. So, it made sense to stay on the Front Range for a bit before making the journey home to the mountains.
- Mount Buckskin (17 May 2020) - May 28, 2020
- Horseshoe Ski (14 May 2020) – The mountain whose journey nearly killed me - May 27, 2020
- Sayres X-Rated Ski (10 May 2020) - May 19, 2020



Wow – incredible. Appreciate all the details and how you worked through the pain with various alternatives, etc . Good job! And it’s great the Universe is smiling on you 🙂 🙂
You got this Brittany. I went through a very similar surgery myself — fused from C5 to T2, from the back. The first few weeks of recovery were the toughest. I know you can recover and will be skiing again! -Brent